A protein electrophoresis is a test that separates blood plasma proteins into different fractions to evaluate the levels of different types of proteins in the blood. It is used to investigate diseases that can cause abnormalities in the amount of proteins circulating in the blood. It is one of the main tests used to diagnose multiple myeloma.
The proteins that are assessed in the electrophoresis are important for the proper functioning of the body. They play a role in immunity, coagulation and metabolism, and are also needed to carry molecules to specific sites within the body. Therefore, abnormal protein levels may be a sign of disease.
Proteins that are tested in an electrophoresis include albumin, alpha-glycoproteins, beta-glycoproteins and gamma-glycoproteins.
What is it used for?
A protein electrophoresis is ordered by the doctor to evaluate the levels of certain proteins in the body. It can help to reach the diagnosis of several conditions and can guide treatment as needed.
Some conditions that may prompt the doctor to order a protein electrophoresis include:
- Dehydration
- Multiple myeloma
- Inflammation
- Cirrhosis
- Systemic lupus erythematosus
- Hypertension
- Ascites
- Glomerulonephritis
- Cushing's syndrome
- Emphysema
- Liver disease
- Anemia
- Pancreatitis
In addition to these conditions, a protein electrophoresis may be advised during pregnancy or for those undergoing estrogen therapy, as both of these situations can alter protein levels.
How it's done
A protein electrophoresis is carried out by collecting a sample of a person's blood, which is then send to the lab. The blood is processed in a way that red blood cells and the plasma are separated, so that protein in the sample can be assessed.
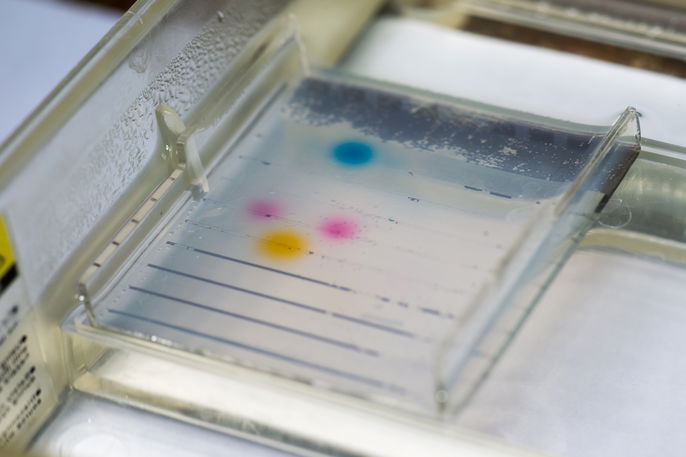
The plasma is placed in an agarose or cellulose acetate gel along with a dye and a marker for each of the proteins. Then, an electrical current is applied to the sample to stimulate the separation of proteins according to their electrical potential, size and molecular weight. Once separated, the proteins can be visualized through a pattern of bands, indicating their presence or absence.
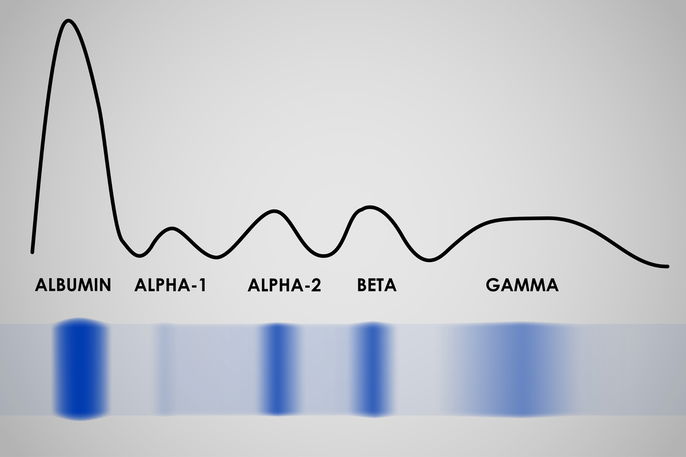
Proteins are quantified in a specific device, called a densitometer, in which the concentration of proteins in the blood is checked. The percentage value and absolute value of each protein fraction is indicated in the ginal report, in addition to a graph.
In some cases, a 24-hour urine collection may be performed to check the amount of proteins released in the urine in a 24-hour period. This test is most often requested by the doctor if kidney problems are suspected.
What results mean
The result of the protein electrophoresis test should be interpreted by the ordering doctor, who will evaluates the absolute and relative values of the proteins in the final report.
The result outlines the protein fractions, or the levels of albumin, alpha-1-globulin, alpha-2-globulin, beta-1-globulin, beta-2-globulin and gamma-globulin.
1. Albumin
Albumin is the plasma protein present in the largest quantities in the blood and is produced in the liver. It performs several functions, such as transporting hormones, vitamins and nutrients, regulating pH levels and controlling osmosis in the body.
Albumin synthesis in the liver depends on the person's nutritional status, hormone levels in the blood and blood pH. Therefore, the amount of albumin in a protein electrophoresis can demonstrate the person's general nutritional status and can flag possible problems in the liver or kidneys.
Also recommended: Albumin Blood Test: High and Low Levels (& What Results Mean) tuasaude.com/en/albumin-blood-testReference value (may vary depending on the laboratory): 4.01 to 4.78 g/dL; 55.8 to 66.1%
High albumin: High albumin levels occur mainly as a consequence of dehydration, but not because there has been an increase in the production of this protein, but because water volume in the blood has become reduced, leading to a higher concentration.
Low albumin: Albumin is considered a negative acute phase protein, which means that in the face of inflammation, albumin will lower. Therefore low levels of albumin can be noted in cases of diabetes mellitus, hypertension, edema, ascites, nutritional deficiencies and cirrhosis.
2. Alpha-1-globulin
The alpha-1-globulin is made up of several proteins, the main ones being alpha-1-acid glycoprotein (AGA) and alpha-1-antitrypsin (AAT). AGA plays a role in the formation of collagen fibers and is responsible for inhibiting the activity of viruses and parasites. Therefore, it plays a fundamental role in the proper functioning of the immune system. Like AGA, AAT is also important for immunity.
Reference value (may vary depending on the laboratory): 0.22 to 0.41 g/dL; 2.9 to 4.9%
High alpha-1-globulin: An increase in alpha-1 globulin occurs mainly with inflammation and infections, and may be a sign of cancer, Cushing's syndrome, arthritis, pregnancy and vasculitis. It can also become high as a result of estrogen or corticosteroid treatment.
Low alpha-1-globulin: A decrease can occur as a result of nephrotic syndrome, severe liver disease, emphysema, cirrhosis and hepatocellular carcinoma.
3. Alpha-2-globulin
The alpha-2-globulin fraction is formed by three main proteins: ceruloplasmin (CER), haptoglobin (hpt) and macroglobulin (AMG). These can become increased with inflammation and infections.
Ceruloplasmin is a protein that is synthesized by the liver and has a large amount of copper in its composition. This allows it to carry out some reactions in the body. Furthermore, CER is important in the process of transforming iron into transferrin, which is the protein responsible for transporting iron in the body. Although it is also considered to be an acute phase protein, CER levels take time to rise.
Haptoglobin is responsible for binding to circulating hemoglobin and promoting its degradation and elimination from the bloodstream. Macroglobulin is one of the largest plasma proteins and is responsible for regulating inflammatory and immunological reactions. It also helps to transport smaller proteins and peptides, and plays a role in the synthesis of plasma proteins in the liver.
Reference value (may vary depending on the laboratory): 0.58 to 0.92 g/dL; 7.1 to 11.8%
High alpha-2-globulin: An increase in alpha-2 globulin may be a sign of nephrotic syndrome, Wilson's disease, liver disease, disseminated intravascular coagulation and stroke. It can also be high as a result of estrogen therapy.
Low alpha-2-globulin: Low levels of this protein can occur due to hemolytic anemia, pancreatitis and lung diseases.
4. Beta-1-globulin
Transferrin is the main protein of beta-1-globulin and is responsible for transporting iron to various parts of the body. While it can be detected on a protein electrophoresis, transferrin levels can also be checked in a normal blood test. Read more about the transferrin test and how it is completed.
Reference value (may vary depending on the laboratory): 0.36 to 0.52 g/dL; 4.9 to 7.2%
High beta-1-globulin: High levels may be the result of iron deficiency anemia, pregnancy, jaundice, hypothyroidism and diabetes.
Low beta-1-globulin: Low levels are not very common, however it can be noted in chronic diseases.
5. Beta-2-globulin
There are two main proteins in the beta-2 globulin: beta-2-microglobulin (BMG) and C-reactive protein (CRP). BMG is a marker of cellular activity, and is important for detecting lymphocyte tumors, infections and inflammation. It can be beneficial for the monitoring of cancer patients
CRP is a very important protein in identifying infections and inflammation, as it is the one of the proteins that undergoes the most fluctuations in its levels. Learn more about C-reactive protein and how it is tested.
Reference value(may vary depending on the laboratory): 0.22 to 0.45 g/dL; 3.1 to 6.1%
High beta-2-globulin: An increase can happen with lymphocyte diseases, inflammation and infections.
Low beta-2-globulin: A decrease may be a sign of liver disease, which prevents the synthesis of these proteins.
6. Gamma globulin
This fraction looks at the immunoglobulins are found, in the sample which are the proteins responsible for the body's defense mechanisms.
Reference values: 0.72 to 1.27 g/dL; 11.1 to 18.8%
High gamma globulin: High gamma globulin can occur with infections, inflammation and autoimmune diseases, like rheumatoid arthritis. Furthermore, there may be an increase in lymphoma, cirrhosis and multiple myeloma.
Low gamma globulin: Low gamma globulin can be a sign of by nephrotic syndrome, gastrointestinal abnormalities that interfere with the absorption of nutrients, blood cancer or the use of immunosuppressive medications, corticosteroids or chemotherapy. This condition can also be congenital.






























